Knee Osteoarthritis Pain
Osteoarthritis (OA) is a degenerative condition that most commonly affects the weight bearing joints such as the knees, hips (See Hip OA) and ankles but can affect any joint in the body. It is the most common form of arthritis and often referred to as “wear & tear” arthritis. OA is the biggest cause of disability in older adults in Australia.
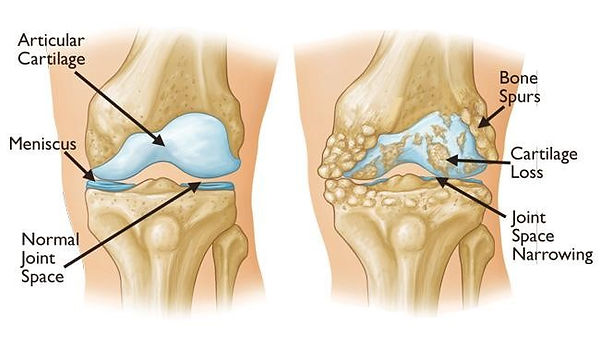
Osteoarthritis affects all the structures that make up a joint, including bone, cartilage, ligaments and muscles. In osteoarthritis, you may get:
-
Inflammation of the tissue around a joint known as the joint capsule
-
Damage to joint cartilage – this is the protective tissue on the ends of your bones which allows your joints to move smoothly
-
Bony growths around the edge of a joint known as osteophytes or spurs
-
Changes to the ligaments, tendons & muscles that support the joint
People of any age can develop osteoarthritis, but it is most common in people over 40 or those who have had previous injuries or surgeries to a joint.
OA that develops slowly and progressively in a previously healthy joint is known as ‘primary’ osteoarthritis; whereas OA that develops in joints that have previously been injured or damaged is called ‘secondary’ osteoarthritis.
Causes
Osteoarthritis is caused by the inflammation, breakdown, and eventually, the loss of cartilage in the joints.
In healthy joints, the ends of the two bones that come together to form the joint (known as the articular surfaces) are covered in a specialised tissue known as articular cartilage. This cartilage is very dense, smooth and slippery and allows for friction free movement and load transmission in the joint, basically acting as padding to prevent the bones from rubbing against each other. Unfortunately, this cartilage does not have a good nerve or blood supply so does not have the ability to heal and repair like other soft tissues. In joints with osteoarthritis, the cartilage becomes damaged which leaves the bones unprotected and vulnerable to further damage, eventually leading to damage & the breakdown of the other tissues in the joint.
Risk Factors
These factors can increase your risk of developing osteoarthritis:
-
Age – OA becomes more common with increasing age.
-
Previous joint injury or damage – Includes infections, fractures, ligament or tendon injuries that can cause instability or alter the biomechanics of the joint often leading to uneven or increased wear
-
Overuse of the joint – For example, osteoarthritis of the hip may be more common in people who have jobs involving repetitive heavy lifting or squatting
-
Overweight / Obesity – Knee and hip osteoarthritis are more likely to develop, or be more severe, in people who are overweight or obese. This is because there is an increased load on the joints
-
Sex – Women are more likely than men to develop osteoarthritis.
-
Family history – There is often a genetic link to certain types of arthritis. This can be due to the shape, size or structure of joints meaning you may be more likely to develop arthritis if other family members have the condition.
Signs & Symptoms
Symptoms of OA can vary from person to person, and also depend on which joints are affected. The signs and symptoms can include:
-
Joint pain worse during and after activity, better with rest (Pain at rest or at night can start as the condition progresses).
-
Joint stiffness, usually worse in the mornings, eased by movement
-
Tenderness on or around the joint
-
Crepitus (Clicking, crackling or grating noises or feelings in the joint)
-
Swelling around the joint
-
Changes to the shape of the joint (Eg bowing of the knees or enlarged joints caused by bony growths)
-
Loss of range of movement
-
Inability to carry out normal activities
Knee OA is characterised by pain after any walking or weight bearing activity, particularly squatting or descending stairs, often accompanied by swelling. There is usually increasing stiffness and loss of ROM as the condition progresses while many patients also report a grating sensation as the knee is moved. Later stage OA knees may start to bow as one side of the joint wears quicker than the other and the patient may report weakness and feelings of instability or giving way.
OA can become very debilitating if left untreated, so it is always best to seek advice as soon as symptoms present.
Diagnosis
The initial diagnosis is often made clinically on the history provided, the presenting symptoms and the physical assessment. It is easily confirmed with X-rays which can give good information on the extent of the damage but are not always required.
Treatment
While the bony changes of OA are not reversible, initial treatment should focus on slowing progression of the disease and allowing the patient to better manage their condition. Some of the biggest strategies here will include education, weight loss if required and the commencing of an exercise program. Exercise programs will usually consist of a mix of home-based strengthening exercises and hydrotherapy which is a great way to strengthen around the joint whilst also reducing the impact and load on knee. Often an early intervention program can prevent the need for further invasive treatments such as surgery.
A recent review of all available scientific evidence found that completing a therapeutic exercise program for OA knee gave significantly reduced pain levels and improved function and quality of life in adults of all ages, immediately after completing a program of 6-12weeks and for at least 12months afterwards.
Manual therapies such as joint mobilisations and soft tissue release techniques may be used in conjunction with the exercise program to provide symptom relief as required.
Surgical Management
In some cases the OA can progress to a point where the pain and disability starts to negatively affect quality of life. In these cases, surgery may be required. Depending on which surfaces of the joint are affected a hemi arthroplasty (half joint replacement eg just the femur or tibia), or more commonly a total knee replacement may be carried out. Whilst fairly major surgeries, these are now very common with over 60,000 total knee replacements performed in Australia in 2017, with the techniques and prosthetics used today also making the procedure much less traumatic than previously. Research shows that both pre-operative and post-operative rehab are important in ensuring the best possible recovery outcomes are met in knee replacement surgeries.


If you think you may be suffering from pain or other knee OA related symptoms, no matter whether it has been for 3 days or 3 decades get in touch today to see how one of our physiotherapists can help you.
